It often starts subtly. Maybe you find yourself getting up more frequently in the middle of the night, a change you might brush off as just “getting older.” Or perhaps you’ve noticed a frustrating delay before urination starts. These small shifts can be easy to ignore, yet they mirror some of the early signs of prostate cancer that health experts advise watching for. For many men, discussing urinary or sexual health feels private, but these are precisely the conversations that matter most. Understanding these signals isn’t about causing alarm; it’s about empowerment.
When you know what to look for, you are better equipped to have an informed conversation with your healthcare provider. This knowledge transforms vague concern into proactive action, which is the cornerstone of maintaining long-term health.
More Helpful Reads You Might Like:
What Is the Prostate and Why Does Its Health Matter?
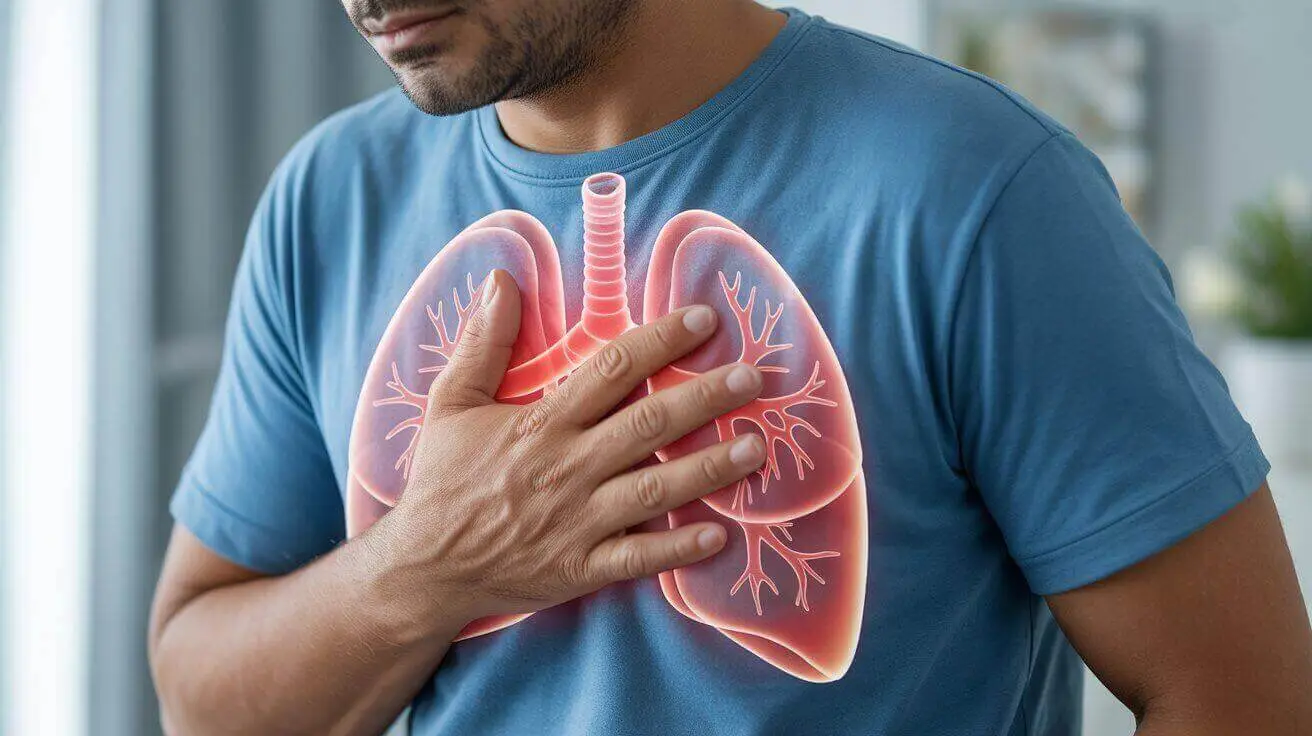
Before diving into symptoms, it’s helpful to understand what the prostate is. The prostate is a small, walnut-shaped gland that is part of the male reproductive system. Its primary job is to produce the seminal fluid that nourishes and transports sperm.
Located just below the bladder and in front of the rectum, its position is key to understanding why its changes can cause such noticeable symptoms. As the prostate gland grows—a common process as men age—it can press on the urethra (the tube that carries urine from the bladder out of the body), interfering with normal urinary function. While this growth is often benign (non-cancerous), a condition known as benign prostatic hyperplasia (BPH), it can sometimes be caused by the development of cancer cells.
Recognizing the Potential Signs and Symptoms
It is crucial to recognize that the early signs of prostate cancer are often subtle or even non-existent, which is why screening discussions with a doctor are so important, especially for those with risk factors. However, as the cancer grows, it may lead to a variety of signs. Many of these symptoms can also be caused by other, less serious conditions like BPH or an infection.
According to leading health organizations like the American Cancer Society, some individuals with prostate cancer may experience the following:
- Common Urinary Symptoms of Prostate Cancer: These are among the most common signs due to the prostate’s proximity to the urinary system.
- A frequent need to urinate, especially at night (nocturia).
- Difficulty starting urination or a weak, interrupted urine stream.
- A feeling that the bladder has not emptied completely.
- Pain or a burning sensation during urination (less common).
- Other Key Signs to Be Aware Of:
- Blood in Urine or Semen: Seeing blood in your urine (hematuria) or semen is a signal that should always prompt a visit to a healthcare professional. While it can have other causes, it should never be ignored.
- Discomfort in the Pelvic Area: Some men may experience a persistent feeling of pain or pressure in the rectum, or a new onset of pain in the lower back, hips, or pelvis.
- Erectile Dysfunction: The new and sudden onset of difficulty achieving or maintaining an erection can sometimes be related to prostate health, although it is more commonly associated with other conditions.
It’s important to approach this list with a balanced perspective. Having one or more of these symptoms is not a confirmation of cancer. Age-related prostate enlargement (BPH) is a far more common cause of urinary issues. However, the only way to know for sure is to consult a doctor.
What Are the Symptoms of Advanced Prostate Cancer?
If prostate cancer is not caught early, it can spread (metastasize) to other parts of the body, most commonly the bones. When this happens, the symptoms can become more systemic and severe. These may include:
- Bone Pain: Persistent, deep pain in the bones, especially in the back, hips, or thighs. This pain may not go away with rest.
- Unexplained Weight Loss: Losing weight without changes in diet or exercise can be a sign of advanced cancer.
- Fatigue: A profound sense of tiredness that isn’t relieved by sleep.
These symptoms warrant immediate medical attention.
When to See a Doctor for Prostate Symptoms
Reading a list of symptoms online can be overwhelming, but a healthcare professional can help you understand if what you’re experiencing relates to the early signs of prostate cancer or a more common condition like BPH. The single most constructive action you can take is to schedule an appointment with your healthcare provider.
A doctor can help you:
- Assess Your Personal Risk: Factors like age, family history, and ethnicity can influence your risk for prostate cancer. A doctor can put your symptoms into the context of your overall health profile.
- Perform an Evaluation: This may involve a discussion of your symptoms, a physical exam (such as a digital rectal exam or DRE), and potentially a blood test to check your Prostate-Specific Antigen (PSA) level.
- Determine the Cause: Based on the evaluation, your doctor can determine if your symptoms are likely due to BPH, an infection, or if further investigation for prostate cancer is needed.
- Create a Plan: Whether it’s “watchful waiting,” medication for BPH, or a referral to a urologist for further testing, having a clear plan reduces anxiety and ensures you are taking the right steps for your health.
A Final Thought on Proactive Health
Your body has a unique language, and learning to listen to it is one of the most powerful things you can do for your well-being. Changes in urinary habits or new discomforts are not just inconveniences to be endured; they are valuable pieces of information.
By treating these signs with gentle curiosity instead of fear, you can take charge of your health narrative. The goal is not to live in a state of constant self-monitoring but to build a partnership with your body and your doctor—a partnership based on awareness, open communication, and proactive care. That is the true path to lasting health and peace of mind.
Medical Disclaimer: This content is for educational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult your physician or a qualified healthcare provider with any questions about a medical condition.
Frequently Asked Questions (FAQ)
I have to urinate frequently at night. Does this automatically mean I should be worried about prostate cancer?
Not at all. Waking up to urinate at night, a condition called nocturia, is very common, especially as men get older. In most cases, it is caused by a non-cancerous enlargement of the prostate known as Benign Prostatic Hyperplasia (BPH) or other factors like fluid intake habits. While it is one of the potential urinary symptoms of prostate cancer, it is far more often linked to BPH. The key is to discuss this change with your doctor, who can help determine the cause and recommend the right course of action, rather than assuming the worst.
Are there any early signs of prostate cancer that are not related to urination?
Yes, although they are less common in the very early stages. Some men might experience persistent pain or discomfort in the pelvic area, lower back, or hips. The new onset of erectile dysfunction or the presence of blood in the semen can also be potential signs. However, because early-stage prostate cancer often has no symptoms at all, relying on symptom-spotting alone is not enough. This is why regular check-ups and an open conversation about your personal risk factors with a healthcare provider are so important.
I have some of these symptoms. Should I ask my doctor for a PSA test immediately?
It’s natural to want a definitive answer, but the best first step is to simply have a conversation with your doctor about your symptoms and concerns. The Prostate-Specific Antigen (PSA) test is a tool, but it’s not perfect and isn’t always the right next step for everyone. Your doctor will consider your age, family history, overall health, and the nature of your symptoms to decide on the most appropriate evaluation. This may or may not include a PSA test. The goal is a shared decision-making process, not a rush to testing.
Can I reduce my risk of prostate cancer through diet or lifestyle?
While there is no guaranteed way to prevent prostate cancer, certain lifestyle choices are associated with a lower risk and support overall health. Research suggests that a diet rich in fruits, vegetables, and healthy fats (like those found in olive oil and nuts) and low in red and processed meats may be beneficial. Maintaining a healthy weight, engaging in regular physical activity, and not smoking are powerful steps for your general well-being and may influence prostate health. Always discuss significant lifestyle changes with your healthcare provider.
Sources & Further Reading
- Prostate Cancer Early Detection, Version 2.2023, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network (JNCCN). https://pubmed.ncbi.nlm.nih.gov/36898362/
- Signs and Symptoms of Prostate Cancer. American Cancer Society (ACS ).
https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/signs-symptoms.html - Prostate Cancer Screening. National Cancer Institute (NCI – part of NIH ).
https://www.cancer.gov/types/prostate/patient/prostate-screening-pdq - Symptoms of Prostate Cancer- Centers for Disease Control and Prevention (CDC ). https://www.cdc.gov/prostate-cancer/symptoms/index.html
- Prostate cancer – Symptoms and causes. Mayo Clinic.
https://www.mayoclinic.org/diseases-conditions/prostate-cancer/symptoms-causes/syc-20353087