It often starts subtly. A forgotten name that used to be on the tip of the tongue. A misplaced set of keys, now a daily scavenger hunt. For millions of families, these small moments of confusion can grow into a cloud of concern, casting a shadow of uncertainty over the future. Watching a loved one navigate the challenges of cognitive decline is deeply personal and often painful. For decades, a diagnosis of Alzheimer’s disease felt like a final verdict, with limited options that only addressed symptoms. But what if the landscape of new Alzheimer’s treatments is finally changing that narrative?
In the last couple of years, the scientific community has reached a monumental turning point. After decades of relentless research, we are witnessing a wave of breakthroughs that are not just promising, but are actively transforming how we approach Alzheimer’s disease. This isn’t about false hope or miracle cures; it’s about tangible, science-backed progress that is offering the first real opportunity to slow the disease’s progression. Let’s walk through what these advances mean, explained in a way that makes sense for you and your family.
More Helpful Reads You Might Like:
Understanding the Shift: From Symptom Management to Disease Modification
For a long time, treatments for Alzheimer’s disease worked by boosting chemicals in the brain that help with memory and thinking. Think of them as a temporary patch—helpful for a while, but unable to stop the underlying damage from getting worse. The core problem in the Alzheimer’s brain involves two key proteins: amyloid-beta, which clumps together to form sticky plaques between nerve cells, and tau, which forms toxic tangles inside them. Together, they disrupt communication between brain cells, leading to their eventual death and the cognitive decline we associate with the disease.
The new era of treatment is exciting because it’s the first to directly target these root causes. Instead of just patching the symptoms, these new therapies are designed to modify the course of the disease itself.
The First Disease-Modifying Therapies: A New Class of Drugs
The most significant news comes from the recent FDA approvals of two groundbreaking medications: lecanemab (brand name Leqembi) and donanemab (brand name Kisunla). These aren’t pills you take every day; they are biologic therapies, known as monoclonal antibodies, administered through intravenous (IV) infusions. These new Alzheimer’s treatments represent the most significant advancement in decades.
Their mission is precise: to seek out and remove the amyloid-beta plaques from the brain. By clearing these sticky clumps, they help restore a healthier environment for brain cells and have been shown in major clinical trials to modestly slow down the rate of cognitive and functional decline in people with early-stage Alzheimer’s disease. The slowdown might be in the range of 27-35%, which, for a family, can mean several more months of preserved independence and quality time.
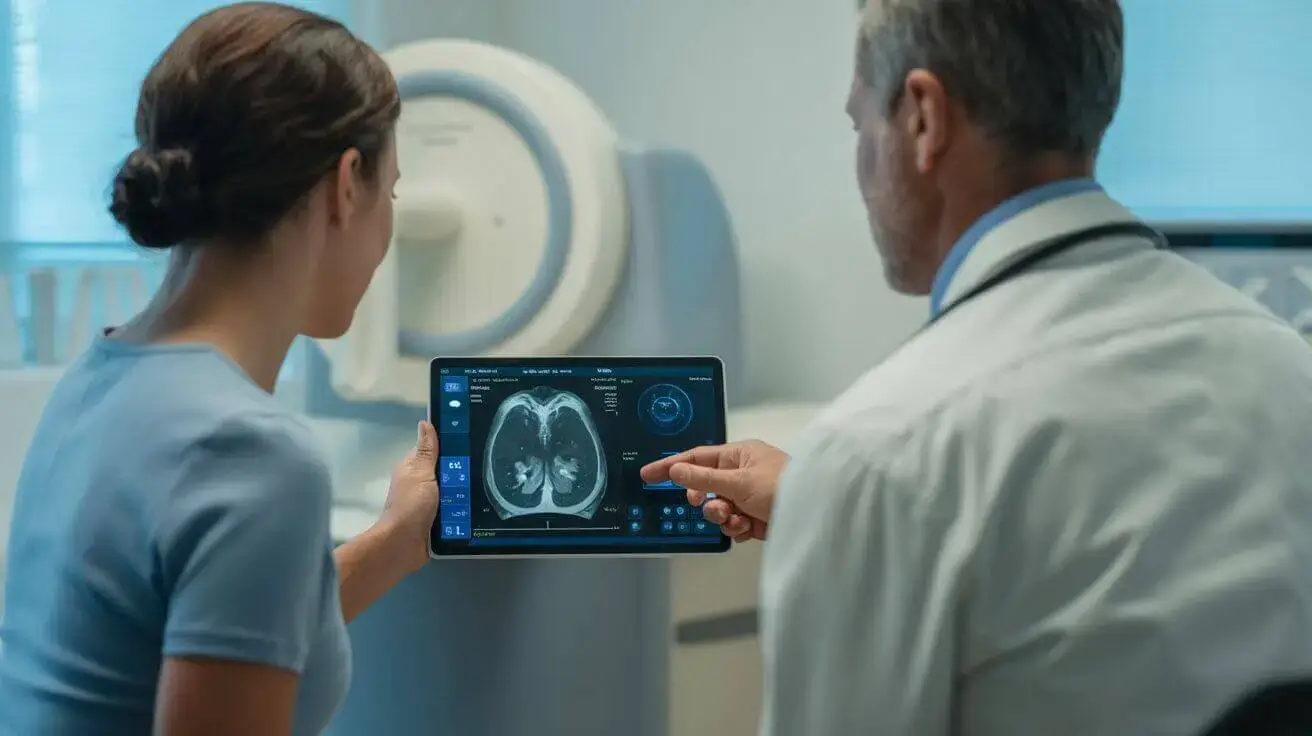
It’s important to have a balanced perspective on these treatments. They are not a cure, and they are most effective for individuals in the early stages of the disease (mild cognitive impairment or mild dementia due to Alzheimer’s). They also come with potential side effects, most notably a risk of brain swelling or micro-bleeds (known as ARIA), which requires careful monitoring with regular MRI scans. A healthcare provider will carefully evaluate if someone is a good candidate for a lecanemab Alzheimer’s treatment, considering their overall health and the specific characteristics of their disease.
A Revolution in Diagnosis: Why a Simple Blood Test Changes Everything
For these new drugs to be effective, early and accurate diagnosis is paramount. In the past, confirming the presence of amyloid plaques in the brain required either a costly PET scan or an invasive spinal tap. This created significant barriers for many people. But in May 2025, another historic milestone was reached: the FDA cleared the first blood test to aid in the diagnosis of Alzheimer’s disease.
This new test, which measures the ratio of specific amyloid and tau proteins in the blood, offers a much simpler, more accessible, and less invasive way to detect the disease’s signature pathology. This diagnostic breakthrough works hand-in-hand with new Alzheimer’s treatments to provide earlier intervention. It provides doctors with a powerful tool to identify who might benefit from the new disease-modifying therapies much earlier in the disease process. This is a critical step toward making personalized Alzheimer’s care a reality for more people, reducing the diagnostic odyssey that many families endure.
Practical Steps and Lifestyle Interventions: What You Can Do Now
While these medical advances are incredibly encouraging, the power of lifestyle choices in supporting brain health remains as important as ever. Evidence consistently shows that proactive steps can help reduce the risk of cognitive decline and support overall well-being. Here are some actionable brain health lifestyle changes grounded in science:
1. Prioritize Heart Health: What’s good for the heart is good for the brain. The brain relies on a rich supply of oxygenated blood, and conditions like high blood pressure, high cholesterol, and diabetes can damage blood vessels and increase dementia risk. Work with your doctor to manage these conditions effectively.
2. Stay Physically Active: Regular physical activity is one of the most effective strategies for protecting brain health. Aim for at least 150 minutes of moderate-intensity exercise per week, such as brisk walking, swimming, or cycling. Exercise increases blood flow to the brain and may stimulate the growth of new brain cells.
3. Adopt a Brain-Healthy Diet: Diets rich in fruits, vegetables, whole grains, lean proteins (like fish), and healthy fats (like those in olive oil and nuts) have been linked to better cognitive outcomes. The Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets are excellent models. Limiting processed foods, sugar, and saturated fats is also key.
4.Challenge Your Mind: Keeping your brain active and engaged helps build cognitive reserve—the brain’s ability to withstand age-related changes. Engage in activities that you enjoy and that make you think: read, learn a new skill or language, play strategy games, or take up a new hobby.
5. Nurture Social Connections: Meaningful social engagement is a powerful protector of cognitive function. Spending time with friends, family, and community groups helps reduce stress and keeps your brain active. Loneliness, in contrast, has been linked to an increased risk of cognitive decline.
6. Prioritize Quality Sleep: Sleep is when the brain clears out toxins, including amyloid-beta. Aim for 7-8 hours of quality sleep per night. If you struggle with sleep apnea or insomnia, seeking treatment is crucial for both your brain and overall health.
A New Horizon of Hope
The journey with Alzheimer’s disease is still challenging, but for the first time in a long time, the path forward is illuminated by genuine, science-driven hope. The arrival of new Alzheimer’s treatments and revolutionary diagnostic tools has fundamentally altered the landscape. We have moved from a place of passive acceptance to one of active intervention. While the road to a cure is still being paved, these breakthroughs mean that for many, the progression of Alzheimer’s may no longer be an unstoppable force. By combining these medical advances with proactive lifestyle choices, we are entering a new era where a diagnosis of Alzheimer’s is not the end of the story, but the beginning of a new, more hopeful chapter.
Medical Disclaimer: This content is for educational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult your physician or a qualified healthcare provider with any questions about a medical condition.
Frequently Asked Questions (FAQ)
1. Are these new Alzheimer’s treatments a cure for the disease?
This is an excellent and important question. Currently, these new breakthrough drugs are not a cure for Alzheimer’s disease. Their primary benefit is to modestly slow down the cognitive and functional decline associated with the disease. Think of it as changing the trajectory of the illness rather than stopping it entirely. They represent a monumental first step in modifying the disease’s course, offering patients more time with preserved function, but they do not reverse existing brain damage or cure the disease.
2. Who is a good candidate for these new monoclonal antibody treatments like lecanemab?
Eligibility for these new Alzheimer’s treatments is quite specific and must be determined by a qualified healthcare provider. Generally, they are intended for individuals in the early stages of Alzheimer’s disease, meaning those with mild cognitive impairment (MCI) or mild dementia who have confirmed evidence of amyloid plaques in their brain. A thorough evaluation, which may include imaging and now potentially an Alzheimer’s blood test diagnosis, is required. A doctor will also carefully weigh the potential benefits against the risks, such as brain swelling or bleeding (ARIA), for each individual.
3. Should I ask my doctor for the new Alzheimer’s blood test?
While the new blood test is a major advancement, it is not intended as a routine screening tool for the general population. It is designed to be used by specialists to help diagnose or rule out Alzheimer’s in individuals who are already experiencing symptoms of cognitive decline. If you or a loved one are noticing persistent memory or thinking problems, the first step is always a comprehensive clinical evaluation. The blood test is one of several tools a doctor might use to understand the cause of these symptoms, not a preventative check-up test.
4. Beyond medication, what is the single most important thing I can do for my brain health?
There is no single “magic bullet” for brain health; rather, the evidence points to the powerful, cumulative effect of consistent, healthy habits. If one area had to be highlighted, it would be managing cardiovascular health. A healthy heart and blood vessels ensure your brain gets the oxygen and nutrients it needs to function optimally. This involves regular physical activity, a balanced diet (like the Mediterranean or DASH diet), and working with your doctor to control blood pressure and cholesterol. Combining these brain health lifestyle changes with social engagement and lifelong learning creates a robust defense against cognitive decline.
Sources & Further Reading
1.PubMed Central (National Library of Medicine): Safety and efficacy of lecanemab for Alzheimer’s disease: a systematic review and meta-analysis of randomized clinical trials
2.National Institute on Aging (NIA): How Is Alzheimer’s Disease Treated?
3.Mayo Clinic: Alzheimer’s treatments: What’s on the horizon?
4.Harvard Health Publishing: The new Alzheimer’s blood test: What it means for diagnosis
5.Centers for Disease Control and Prevention (CDC): Reducing Risk for Dementia