Have you ever woken up on a chilly, cloudy morning and felt that familiar ache in your knees, hips, or hands? Maybe you’ve joked that you can “predict the rain” better than the forecast. You’re not alone—many people notice a clear link between joint pain and weather changes. But is this just an old wives’ tale, or does science actually back it up?
Let’s explore what really happens inside your body when the weather shifts—and how you can manage that discomfort if you’re one of those “human barometers.”
More Helpful Reads You Might Like:
The Weather–Joint Pain Connection: Myth or Reality?
For decades, scientists have studied the relationship between weather and joint pain, especially in people with arthritis. While research results have been mixed, a growing number of studies support what many people already know from experience—changes in weather, especially in barometric pressure, temperature, and humidity, can affect joint pain.
So no, you’re not imagining it. The connection may be subtle, but it’s real for many people.
How Barometric Pressure Affects Your Joints
The most common explanation involves barometric pressure, which is the weight of the air pressing on the earth (and on you). When the weather shifts—especially before it rains or gets colder—barometric pressure drops.
Here’s what that means for your body:
- Your tissues expand slightly. Lower air pressure gives body tissues (like tendons and muscles) a little more room to swell. Even a small amount of swelling can put pressure on nerves in or around the joints, triggering pain.
- Inflamed joints are extra sensitive. If you have arthritis, your joint linings (synovium) are already inflamed and more reactive. Changes in pressure can amplify that irritation, making joints feel stiffer or achier.
- Joint fluid thickens in cooler weather. Synovial fluid—the natural lubricant inside your joints—can become thicker in cold temperatures, making it harder for the joint to move smoothly. That stiffness can contribute to pain.
In short, when barometric pressure drops, your joints might “feel” the change before your eyes can see it in the sky.
Temperature and Humidity Also Play a Role
It’s not just pressure. Temperature and humidity swings can also influence how your joints feel:
- Cold weather: Cooler temperatures can cause muscles to tighten and blood flow to slow slightly, making joints stiffer. That’s why you may feel more aches in winter or after stepping out into a cold wind.
- High humidity: Damp air can increase joint stiffness and discomfort, especially when combined with heat or sudden weather changes.
- Rapid fluctuations: The biggest culprit may not be the absolute temperature or humidity, but how quickly they change. Your body often struggles to adapt to those sudden shifts.
Who’s Most Likely to Feel Weather-Related Joint Pain?
While anyone can feel achy during weather changes, certain groups are more sensitive:
- People with osteoarthritis (the “wear and tear” type of arthritis)
- Those with rheumatoid arthritis (an autoimmune condition that causes joint inflammation)
- People with fibromyalgia or chronic pain syndromes
- Older adults—because joint cartilage tends to thin and nerve endings may become more reactive with age
However, even young, healthy people sometimes report mild joint discomfort before storms or during cold snaps. Your body’s connective tissues are living, responsive systems—they don’t exist in isolation from the environment.
What Science Says: Key Research Findings
Scientific evidence for weather-related joint pain isn’t black and white, but several high-quality studies have found significant links:
- A 2019 study in Pain (McAlindon et al.) found that people with knee arthritis reported increased pain on days with falling barometric pressure and rising humidity.
- A Harvard-affiliated study (Zhou et al., 2018) also noted that joint pain reports rose with lower atmospheric pressure and higher humidity.
- Conversely, some studies haven’t found a strong correlation, likely because weather effects vary between individuals and depend on local climate and personal sensitivity.
Bottom line: while weather changes don’t cause arthritis or joint disease, they can aggravate symptoms in people who already have underlying joint inflammation or sensitivity.
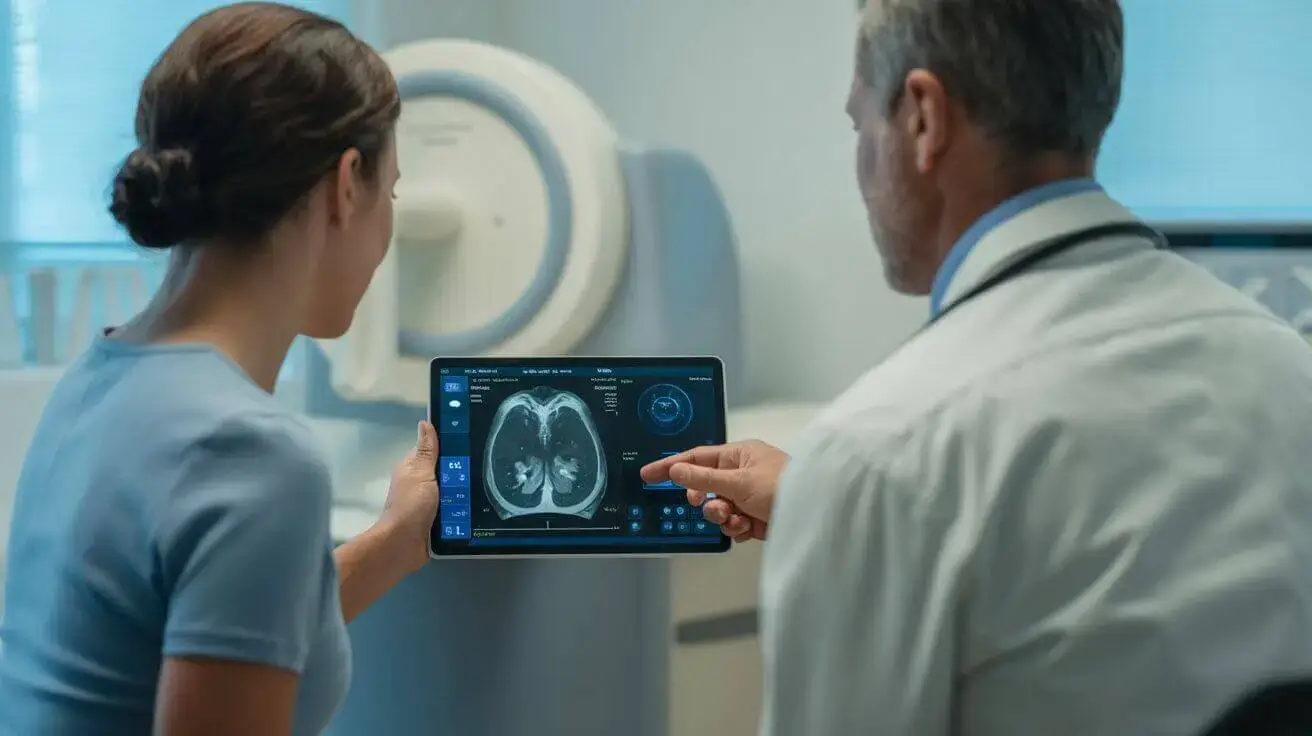
What’s Actually Happening Inside Your Joints
Let’s break down the basic biology in simple terms:
- Your joints are cushioned by cartilage and filled with synovial fluid, which keeps everything moving smoothly.
- Around that fluid is the synovial membrane, a thin lining that produces the fluid and contains nerve endings.
- When air pressure drops or humidity rises, that lining can swell just a bit—enough to stretch the joint capsule and trigger those nerve endings.
- Cold temperatures then cause surrounding muscles and ligaments to contract, increasing stiffness and restricting motion.
Together, those effects explain why your knees or fingers might feel tight, sore, or even a little “creaky” when the weather turns.
Managing Weather-Related Joint Pain
If you’re someone who feels like your joints are mini weather stations, the good news is there are plenty of ways to ease the discomfort.
1. Stay Warm and Keep Moving
Cold, stiff muscles and joints feel worse when you’re inactive. Gentle movement boosts blood flow and keeps synovial fluid circulating. Try:
- Light stretching or yoga indoors
- Low-impact exercises like walking, swimming, or cycling
- Warm showers or heating pads to soothe stiff joints
2. Dress for the Weather
Wear layered, loose-fitting clothing that traps body heat. Gloves, knee sleeves, or thermal socks can help insulate vulnerable joints.
3. Maintain a Healthy Weight
Extra weight puts added pressure on weight-bearing joints (knees, hips, spine), which can worsen discomfort—especially when weather changes.
4. Use Anti-Inflammatory Strategies
Over-the-counter pain relievers like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can help, but always check with your healthcare provider first.
Eating an anti-inflammatory diet—rich in fruits, vegetables, omega-3 fats (like salmon), and whole grains—can also help calm chronic inflammation.
5. Keep Track of Patterns
Some people find it helpful to track joint symptoms alongside local weather data. You might discover that humidity spikes or cold fronts consistently trigger pain—helping you prepare ahead of time.
When to See a Doctor
Weather-related aches are usually mild and temporary. But if you experience:
- Persistent or severe pain
- Swelling, redness, or warmth in a joint
- Pain that limits your daily activities
…it’s time to check in with a healthcare professional. You may be dealing with arthritis or another underlying condition that can be managed with medical care.
A Warm Outlook
While you can’t change the weather, you can take charge of how your body responds to it. Understanding why your joints ache when a storm’s coming empowers you to move more, warm up faster, and care for your joints year-round.
So next time your knees start “forecasting rain,” take it as your body’s gentle reminder to stretch, stay cozy, and keep moving—no umbrella required.
Medical Disclaimer: This content is for educational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult your physician or a qualified healthcare provider with any questions about a medical condition.