You’ve probably seen headlines about vitamin D being the “sunshine vitamin” that could help fend off all kinds of diseases—including breast cancer. It’s natural to wonder: should I be taking vitamin D to lower my risk?
Vitamin D 101: What It Is and How your body uses it
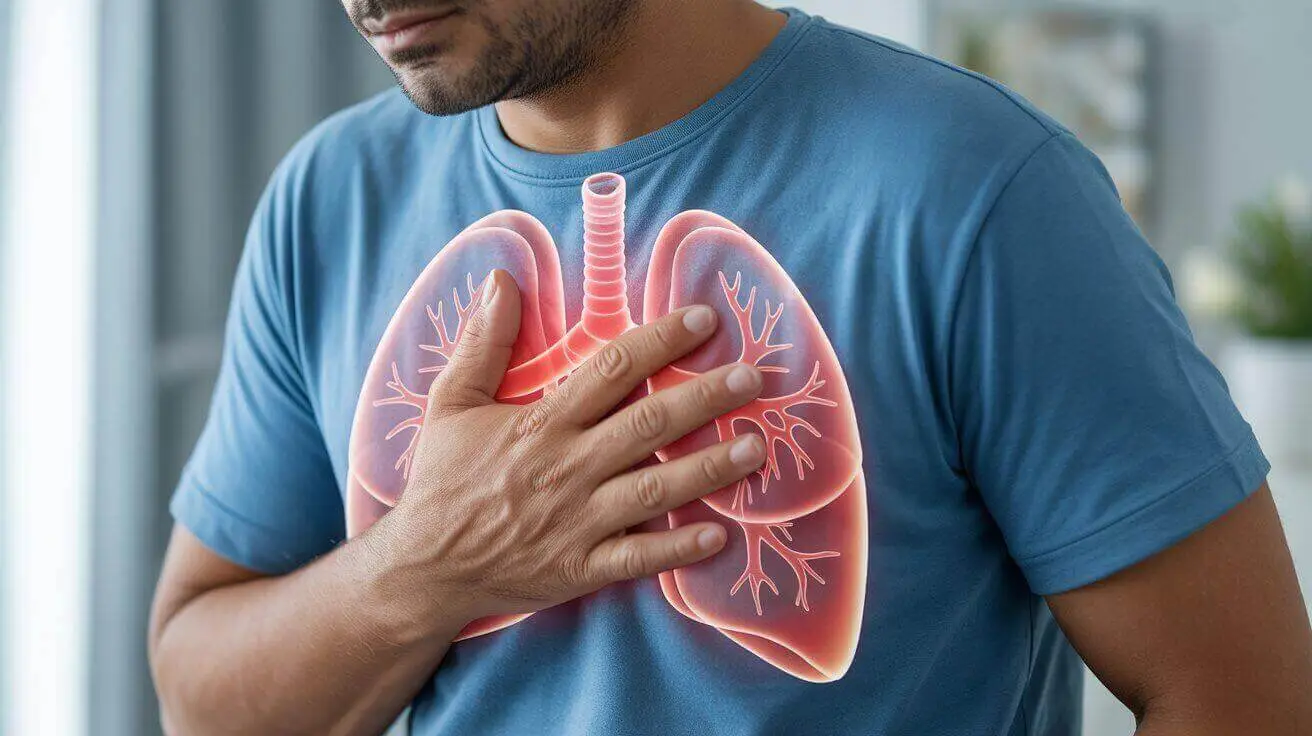
Vitamin D acts more like a hormone than a typical vitamin. Your skin makes it from sunlight; you can also get it from foods (like fortified milk and fatty fish) and supplements. Once vitamin D enters your body, your liver converts it to 25-hydroxyvitamin D [25(OH)D], the main “storage” form we measure on blood tests. Then your kidneys (and some other tissues) convert 25(OH)D into calcitriol, the active form that binds to the vitamin D receptor (VDR) inside cells. When calcitriol flips that VDR “switch,” it can influence hundreds of genes that guide how cells grow, divide, specialize, and die—processes that are central to cancer biology.
Why this matters for cancer biology
In lab and animal studies, vitamin D signaling can:
- Slow down uncontrolled cell growth (proliferation)
- Encourage damaged cells to self-destruct (apoptosis)
- Reduce inflammation
- Interfere with the formation of new blood vessels that feed tumors (angiogenesis)
These are biologically plausible ways vitamin D could help prevent cancer or slow its progression. But what happens in a petri dish doesn’t always translate to human health outcomes—which is why we rely on large, well-done clinical trials to know what actually helps people.
More Helpful Reads You Might Like:
- 7 Reasons to Include Limes and Lime Juice in Your Diet
- Can a Single Protein Reverse Brain Shrinkage? What Science Really Says (and What You Can Do Now)
- Could Kefir Be the Key to Enjoying Dairy Again?
- That Midnight Snack Craving: Could Grapes Be the Secret to Better Sleep?
- Beyond the Pain: A Practical Guide to Kidney Stone Prevention
So… Does Vitamin D Prevent Breast Cancer?
Observational studies vs. randomized trials
For years, observational studies (which watch what happens to people who already have certain vitamin D levels) suggested that people with higher blood levels of 25(OH)D might have lower risks of some cancers. But observational studies can be confounded by lifestyle: people with higher vitamin D often spend more time outdoors, exercise more, and have different diets—all of which can lower cancer risk.
When we look at randomized controlled trials—the gold standard—results are more sobering. The largest to date, the VITAL trial (nearly 26,000 U.S. adults taking 2,000 IU of vitamin D3 daily or placebo), found no reduction in total invasive cancer incidence among those assigned to vitamin D versus placebo. In other words, taking vitamin D did not make people less likely to be diagnosed with cancer overall. Breast-cancer–specific prevention benefits were not demonstrated.
The National Cancer Institute sums it up this way: research to date has not shown a consistent association between vitamin D levels and breast cancer risk. That means we don’t have reliable evidence that higher blood levels of vitamin D protect women from developing breast cancer.
A Wrinkle: Advanced Cancer and Cancer Mortality
Here’s where things get interesting. While vitamin D supplementation hasn’t reduced cancer incidence (the number of people who develop cancer), some research suggests it might lower the risk of developing advanced/metastatic cancer and reduce cancer mortality (the risk of dying from cancer).
- A secondary analysis of the VITAL trial reported fewer cases of metastatic or fatal cancer in participants taking vitamin D3, with the strongest signal in people with a normal BMI (body mass index). This finding is hypothesis-generating—it suggests vitamin D might matter more in certain groups—but it’s not definitive proof.
- Multiple meta-analyses pooling many trials have found that vitamin D supplementation is associated with lower cancer mortality (roughly a 13–16% reduction), while still showing no reduction in cancer incidence. That is, vitamin D doesn’t seem to stop cancers from appearing, but it might help people live longer after a cancer diagnosis. The exact mechanism isn’t settled.
These results are encouraging but not ironclad. Meta-analyses are only as strong as the trials they include, and not all trials were designed to examine breast-cancer–specific outcomes. Still, the mortality signal keeps showing up, which is why researchers are continuing to study who benefits most, at what doses, and for how long.
What about people with overweight or obesity?
Vitamin D is fat-soluble, meaning it can get “sequestered” in body fat. Several analyses, including VITAL follow-ups, suggest that BMI may modify the effect of supplementation: people with normal BMI appeared to glean more benefit for advanced cancer endpoints than those with overweight or obesity. One theory is volumetric dilution—the same dose yields lower effective concentrations in people with more adipose tissue. This doesn’t prove cause and effect, but it’s a plausible explanation worth further study.
It’s important to note: As of now, guidelines from the American Cancer Society (ACS) and the National Cancer Institute (NCI) do not recommend adjusting vitamin D dosage based on BMI for cancer prevention — but both organizations acknowledge that BMI may influence serum levels and biological effects.
Where major medical organizations stand—right now
- NIH/Office of Dietary Supplements (ODS): The latest NIH fact sheet concludes that most research has not found a relationship between 25(OH)D blood levels and overall cancer risk, and trials have not shown that supplementation reduces cancer incidence.
- National Cancer Institute (NCI): NCI’s vitamin D and cancer overview states there’s no consistent association between vitamin D and breast cancer risk, and vitamin D supplements have not been shown to reduce cancer incidence, including in large trials like VITAL.
In plain terms: reputable U.S. sources do not currently recommend vitamin D supplements specifically to prevent breast cancer.
Practical ways to keep your vitamin D in a healthy range
- Smart sun: Sunlight helps your body make vitamin D naturally, but safety comes first. According to U.S. dermatology and endocrinology societies, brief sun exposure—about 5 to 15 minutes on most days of the week, to small areas like the face, arms, or legs—can help maintain healthy levels, depending on your skin tone and where you live. Try to get this light exposure in the morning or late afternoon, when UV rays are less intense. Always protect your skin from burns and long-term damage with sunscreen, shade, and protective clothing. If your sun exposure is limited, talk with your healthcare provider about checking your vitamin D levels.
- Food first: Fatty fish (salmon, mackerel, sardines), egg yolks, and fortified foods—such as milk, plant milks, yogurts, and cereals—can all contribute meaningful amounts of vitamin D. These foods help support healthy levels, especially when sun exposure is limited.
- Test and supplement only if needed: The only way to know your vitamin D status is through a blood test. Your healthcare provider can interpret your results and decide whether supplementation is necessary, and what dose is safe for you. Avoid self-prescribing or taking high doses without medical supervision.
If I’ve Had Breast Cancer: Should I Aim for Higher Vitamin D Levels?
It’s common to find low vitamin D levels at diagnosis, and your oncology team may check and treat deficiency for bone and general health—especially if you’re on aromatase inhibitors, which can affect bone density. However, there’s no consensus that pushing vitamin D levels above the usual sufficiency range prevents recurrence. Ensuring sufficiency is sensible; “the higher, the better” is not supported and may carry risks such as high calcium levels and kidney stones if over-supplemented. Always loop in your oncology and primary care teams before starting or escalating supplements.
A Warm Word to Close
Health headlines can be confusing, especially when the message seems to change year to year. You don’t have to figure this out alone. If you’re worried about vitamin D or breast cancer risk, ask your clinician about a simple blood test, your personal RDA, and whether a modest daily supplement makes sense for you. Small, steady steps—getting outside safely, eating well, moving your body, keeping up with screenings—add up over time. You’ve got this, and your care team can help tailor a plan that fits your life.
References
- National Cancer Institute (NCI). Vitamin D and Cancer (updated May 9, 2023). Summary of evidence on vitamin D status, supplementation, and site-specific cancer risks, including breast cancer. National Cancer Institute (NCI)
- Manson JAE, et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. New England Journal of Medicine. 2019;380:33–44. Primary results from the VITAL randomized trial showing no reduction in total invasive cancer incidence with vitamin D3 supplementation. New England Journal of Medicine+1
- Chandler PD, et al. Effect of Vitamin D3 Supplements on Development of Advanced Cancer: A Secondary Analysis of the VITAL Trial. JAMA Network Open. 2020;3(11):e2025850. Reports fewer metastatic or fatal cancers with vitamin D, especially among participants with normal BMI. JAMA Network
- Zhang Y, et al. Association between Vitamin D Supplementation and Total Cancer Incidence and Mortality: A Systematic Review and Meta-analysis of Randomized Controlled Trials. BMJ. 2019;366:l4673. Vitamin D supplementation associated with reduced cancer mortality but not incidence. BMJ+1
- NIH Office of Dietary Supplements (ODS). Vitamin D—Health Professional Fact Sheet (updated June 27, 2025). Includes current RDAs, upper intake levels, and an evidence summary regarding cancer outcomes. NIH Office of Dietary Supplements (ODS)